An ambitious healthcare reform in Colombia may be facing its toughest challenge yet: the pharmaceutical industry.
In a bold step with wide repercussions for Latin America’s healthcare sector and drug patent law, Colombia’s Ministry of Health in late April moved to unilaterally end Swiss drug giant Novartis’ patent on the expensive cancer treatment Glivec after the company refused to sell it at lower cost. This would be the country’s first-ever “compulsory license,” which is when a government allows generic drug production without consent from the patent owner.
The move could reportedly save Colombia tens of millions of dollars annually at a time when the government is struggling to rein in the ballooning costs of expanded healthcare coverage. Perhaps more concerning to the pharmaceutical industry, it could also open the door to further disputes between Latin American governments and drug companies over access to high-cost medicines.
“The Colombian healthcare system is unique and in many ways ahead of most other countries in the region,” Jaime Arias, executive director of the Colombian Association of Medical Companies (ACEMI), told AQ. “What happens here will have an impact on policymaking in the region.”
A spokesperson for Novartis told AQ that it is working with the Health Ministry “to find a mutually beneficial solution” to the dispute, which now lies with Colombia’s superintendent for industry and commerce. The spokesperson added that compulsory licenses should not be used in a threatening manner to force down prices, which “would create a damaging precedent that could apply to all patent-covered innovations.”
The standoff has been brewing for months. In a sense, it can be traced back to President Manuel Santos’ signing in February 2015 of the new Statutory Health Law, which defined healthcare as a fundamental right for all Colombians. Patients became entitled to any drug or treatment licensed in Colombia, doctors were given total freedom of prescription, and hospitals could no longer refuse to treat anyone lacking insurance papers.
Who will pay for that expanded coverage is another question – and is the key factor behind the Health Ministry’s request now for a compulsory license for Glivec (spelled Gleevec in the United States and Canada). Expanded drug coverage has placed a huge financial strain on the healthcare industry, which had accumulated debts of more than $4 billion by the end of 2015, according to data from ACEMI. The Ministry of Health, in its worst-case-scenario, projects the February 2015 law to stick an additional $700 million on its annual pharmaceutical bill. But that may be optimistic, according to Oscar Andia, vice president for pharmaceutical policy for the Colombian Medical Federation.
“The ministry has simply pulled these figures out of a hat,” Andia told AQ. “If patients are given unrestricted access to high cost drugs the total bill will be a lot higher than the government anticipates.”
That’s unless drug prices also come down, as Health Minister Alejandro Gaviria is attempting to make happen. His move to issue a compulsory license represents a 180-degree turn from the previous administration’s open market policies that led to what Andia calls “an orgy of profit for the pharmaceutical industry.” In 2012, the price of Rituximab, a leukemia drug, was found to be 12 times more expensive in Colombia than in the United Kingdom. Interferon beta-1b, used in the treatment of multiple sclerosis, was listed at prices 32 times higher than in the EU.
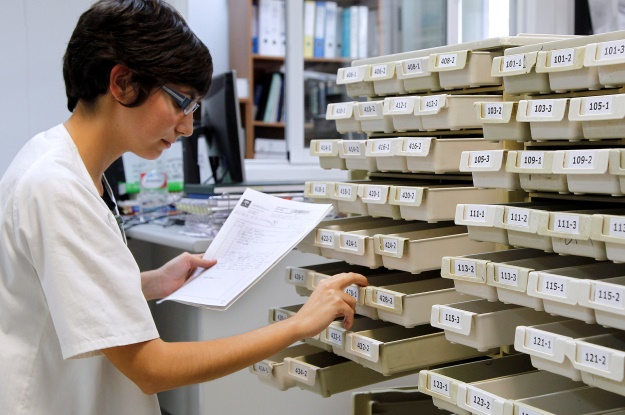
To tackle spiraling costs, the Health Ministry in September 2013 introduced a new price controls policy requiring drug prices to fall into the 25th percentile based on international price referencing of comparable countries. The measure was introduced for 189 key drugs and is continuously expanding. Cost controls have been matched with legislation regarding biosimilars drugs, which are cheap like generic drugs, but created through a different process of protein engineering.
When it came to Novartis, Gaviria first proposed the firm halve the cost of Glivec (also referred to as imatinib) to 140 pesos per milligram – the price offered by generic competitors operating in the country until 2012, when Novartis’ patent was approved. Novartis rejected the offer on April 20, and on April 26 the Health Ministry announced its intention to request the compulsory license.
The World Trade Organization allows a country to cite a health emergency as reason for issuing a compulsory license, as Brazil and India did to bring down the cost of AIDS treatments in the mid-2000s. But it is unclear if this condition is met by the need of Glivec to treat chronic myelogenous leukemia (CML), a cancer of white blood cells affecting about 3,000 Colombians.
“In terms of number of patients, it is hard to say that CML represents a healthcare emergency in Colombia,” said Arias of ACEMI. “However, it could be argued that the high cost of treatment of CML and other diseases places a financial burden on the system that represents a health emergency.”
Approval of the compulsory license from Colombia’s superintendent of industry and commerce was initially considered a matter of protocol, as Gaviria has received strong cabinet support for his wider health reform. But opposition is reportedly coming from both the superintendent and the trade minister, who fear the license could provoke Novartis to litigate for breach of intellectual property clauses in Colombia’s free trade agreement with Switzerland. Colombia was already hit in March with multibillion-dollar lawsuits from two Canadian-owned mining firms under investment protection clauses contained in the free trade pact with Canada.
It is unknown when a decision might be made, but there is still time for Novartis and the ministry to reach agreement on a price for Glivec and avoid a lengthy and costly legal process that neither side wants. No matter the result, Colombia’s threat to issue a compulsory license has the potential to embolden other Latin American nations to consider doing the same, especially if the progressive healthcare reform continues to gain traction as a regional model.
“The dispute shows that Latin American ministries of health can take actions to make the pharmaceutical industry think twice about high prices,” said Claudia Vaca, a former adviser in Colombia’s Health Ministry. “Whatever the outcome, the debate will draw attention to the issue of drug prices and the content of intellectual property legislation, including its flexibilities, in trade agreements.”
—
Youkee an independent journalist and analyst based in Bogotá. Follow him on Twitter: @matyoukee.